Deanna’s Discoveries: Tools to help make tough treatment choices
[anvplayer video=”4593597″ station=”998131″]
ROCHESTER, N.Y. (WHEC) — Studies show that patients who are actively involved in their care, do better and feel better.
There are many reasons for this.
These patients often seek out better care and take better care of themselves, carefully following doctors’ instructions.
But research is difficult, especially when your life is on the line.
Patients are thrust into a world full of medical jargon, odd acronyms, and drugs with multi-syllabic names.
But after facing the ‘Big C’ four times, I’ve come to the conclusion that I must work for my wellness.
After a great deal of research, I decided on a complicated radiation regimen only available at a couple of cancer centers in the country.
While Sloan Kettering is closer to home, I chose MD Anderson Cancer Center in Houston because I have friends and family in Houston who provided a great deal of support while I was there.
By week five of my daily radiation treatments, my skin had begun to show the effects.
I had radiation dermatitis – temporary skin reactions to radiation therapy.
"While it looks bad to the eye, I don’t have patients that are in pain," said Dr. Eric Strom, my radiation oncologist at MD Anderson.
Instead, it itches. That’s certainly true in my case. Dermatitis and fatigue were the only side effects of this complex radiation treatment for my advanced breast cancer.
"You had some disease in the lymph nodes that were underneath the breast bone, so I had to get dose [radiation] there," said Dr. Strom, explaining his treatment approach. "The heart is directly below that, just a couple of centimeters away."
So Dr. Strom created a specialized plan that targeted the tumor beneath my left breast, lymph nodes beneath my breast bone, as well as microscopic cells that could be lurking in my neck and armpit – all while avoiding my heart and lungs.
At every radiation treatment, I had a little bit of home with me, a radiation cape made for me by another survivor at the Breast Cancer Coalition of Rochester.
It brought comfort while getting treatment more than a thousand miles from home.
Radiation therapy technicians carefully checked my position, assuring that I was perfectly aligned. Then my work would begin.
"Take a breath in and hold," the technician directed.
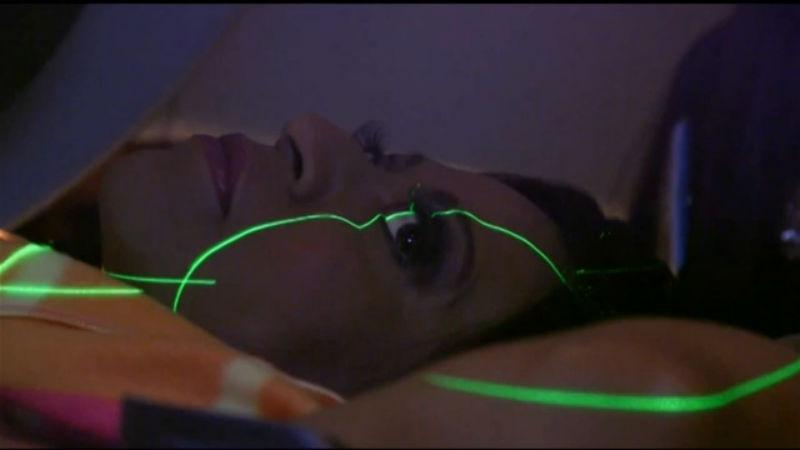
A monitor on my stomach allowed me to gauge how deeply to inhale. I’d watch a monitor with a yellow line that would move up when I inhaled and down when I exhaled.
When I had inhaled enough air in my lungs to separate my heart a safe distance from the radiation target area, the machine would send electrons and photons into the malignant tumor. The technique is called deep inspiration breath-hold or DIBH.
"The breath hold allows your heart to pull away from the area that we’re interested in," Dr. Strom explained.
And that protects the heart from radiation exposure.
This technique is used with patients, like me, who have breast cancer on the left side.
Technicians used electrons above my breast bone, beams that don’t penetrate as deeply as x-ray beams.
That minimized exposure to my heart and lungs. And that’s really important, especially in my case.
I’ve had cancer four times.
Clearly, I have a propensity for developing the disease. And some types of radiation treatment can expose healthy tissue – causing a new cancer years later.
"We’re worried about second malignancies, lung cancers, breast cancers." Dr. Strom explained.
So I did a great deal of research to find this specialized treatment approach for my advanced breast cancer.
"I expect you to be cured, and I don’t expect to have caused you any increased risk for second malignancies in the decades that are to come for you," Dr. Strom told me.
His assurances are comforting. After all, I have a lot to live for.
I’ve chosen to follow my oncologist’s recommendation and take oral chemotherapy following radiation.
Studies show patients with my type of metastatic breast cancer that did not completely respond to initial chemotherapy reduce their chances of recurrence when they follow radiation with another round of chemo.
When making your own choices about treatment, have an honest discussion with a medical team you trust.
Don’t be afraid to get a second opinion, and consider consulting with a specialist from the Cancer Support Community, a non-profit organization that provides psycho-social support to cancer patients and those who love them.
CSC has a program called Open to Options.
You can speak with a Cancer Support Community specialist who will help you explore your options and prepare questions to ask your oncologist.
The Rochester chapter of CSC is Gilda’s Club of Rochester which provides a number of support services for patients.
I also strongly suggest breast cancer patients connect with the Breast Cancer Coalition of Rochester.
BCCR is a non-profit that provides support services and educational seminars that are incredibly helpful when making tough treatment choices.
In the interest of full disclosure, I should mention that in the past I served on the board of CSC of Central Indiana and I currently serve on the Advisory Board of BCCR.
While we, as patients, should always look to our team of professionals for guidance, ultimately the decisions are ours.
And embracing that is empowering.